At the invitation of the Association of Community Mental Health Centers of Kansas, BHECON, the National Council for Behavioral Health and the USC Schaeffer Center for Health Policy and Economics took part in the August 9th convening of the Kansas Mental Health Task Force in Topeka.
The Kansas Cost of Mental Illness Chartbook is being presented to the Mental Health Task Force today thanks to @BHEconNetwork. #ksleg pic.twitter.com/QpXznqh5cC
— ACMHCK (@ACMHCK) August 9, 2018
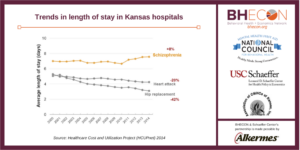
The Mental Health Task Force is a multidisciplinary group commissioned by the state to prioritize additional behavioral health system changes as recommended in its 2017 report. Setting the stage for the Task Force’s discussion, Seth Seabury, PhD presented the updated Kansas 2018 Data Chartbook for its consideration. Dr. Seabury focused in on data related to hospitalization rates, lengths of hospital stay, associated costs of treating mental illness, and costs associated with serious mental illness treatment in jails and prisons to illustrate some of the issues that Kansas faces as it considers policy changes related to its behavioral health system.
The Task Force is currently most interested in correlating causal impacts with the data, for example understanding if longer rates of hospital stays from a schizophrenia-induced admission is due to the treatment received or a lack of available community supports upon discharge of a patient. Causal information is a key element of proving return on investment in behavioral health spending, as savings are often disbursed among multiple social services and over the course of an individual’s lifetime.
The post-presentation discussion illustrated many of the current barriers experienced in behavioral health data collection. When asked whether data is available on specific population subsets with serious mental illness, Dr. Seabury explained that due to privacy concerns, certain demographics are stripped from publicly available datasets. When attempting to dive into county level spending and data, often there are multiple barriers in comparing data due to the collection standards and metrics. Definitions and requirements vary at both the state and county level, often making meaningful comparisons difficult.
A key area of interest for further study is the impact of increased safety net spending in surrounding states on the behavioral health workforce of Kansas. While it is often difficult to compare behavioral health and addiction specific roles across state lines due to differences in licensure requirements and reporting, the Task Force is concerned that increases in safety net spending within Missouri, Colorado, and Oklahoma may be resulting in a depletion of available mental health professionals in Kansas.
The next public meeting of the Kansas Mental Health Task Force will take place in September at the Kansas Institute of Health.
